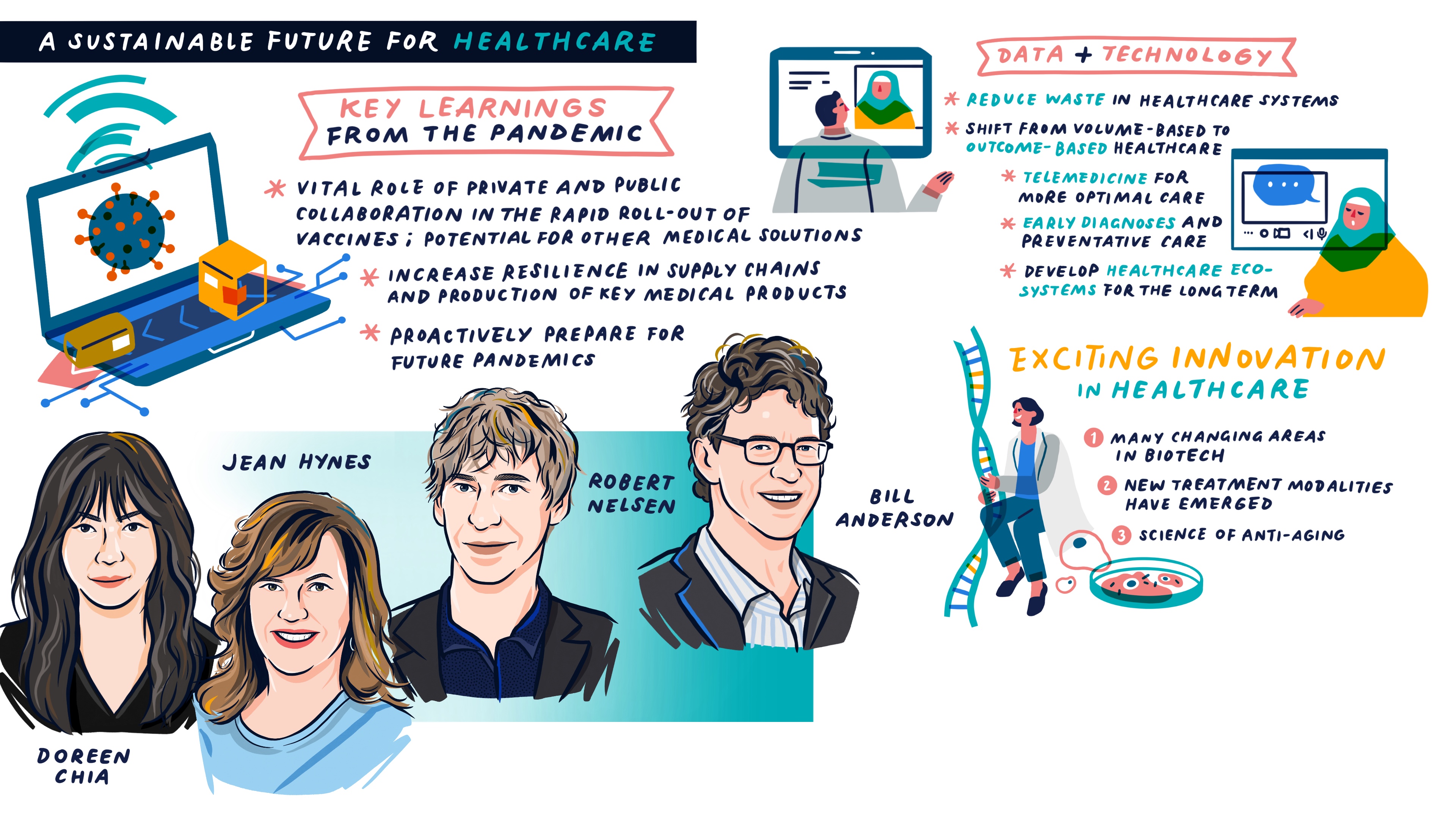
This article summarises a panel discussion at GIC Insights 2021 with Jean Hynes, CEO of Wellington Management; Robert Nelsen, Co-founder and Managing Partner of ARCH Venture Partners; and Bill Anderson, CEO of Roche Pharmaceuticals.
Moderated by Doreen Chia, Managing Director and Chair of GIC’s Healthcare Business Group, the panel spoke about the lessons learnt from Covid-19 that could enable better preparedness for future pandemics, and how innovation could be used to help sustain healthcare systems over the long term.
Dealing with future pandemics
One key positive outcome arising from the Covid-19 crisis was the seamless collaboration between the private and public sectors on the research and development of diagnostics, vaccines and therapeutics. This has resulted in the unprecedented global roll-out of several powerful vaccines in less than a year, a process which typically takes 10 years. Being able to apply a similar approach to future pandemics or even areas like oncology could lead to the development of other significant medical solutions.
Other lessons discussed by the panel included the need to invest more in the domestic production of medical products and their supply chains. Governments need to proactively prepare for the inevitable next pandemic, as future outbreaks could stem from unexpected sources and be even more devastating.
Innovation in the healthcare industry
The panel observed that the healthcare industry was going through an exciting period of rapid innovation and change. There are now many more private companies relative to public companies. Previously, to be a successful investor in biotech, one needed to have knowledge of at least 15 changing areas of medicine, but this has now increased to 50 to 60. While there is significant competition with more capital targeting the sector, there are also a lot more opportunities.
Before the 1990s, there were only small-molecule drugs like Aspirin or Advil. The birth of the biotech industry in the 1990s led to the development of protein drugs and monoclonal antibodies. And in this decade, new treatment modalities have emerged including cell therapy, gene therapy, gene-editing, siRNA (small interfering ribonucleic acid) and mRNA (messenger RNA). The panel was hopeful that a lot of biological problems could be solved in the coming years meaning more advances for patients. Also, because these new modalities are less easy to genericise than small molecules, the industry’s revenue streams are likely to be more durable over the next 10 or 15 years. Another area of investor interest is the science of anti-aging including cellular rejuvenation and epigenetic reprogramming.

“There is a need to invest more in the domestic production of medical products and their supply chains. Governments need to proactively prepare for the inevitable next pandemic, as future outbreaks could stem from unexpected sources and be even more devastating.”
New care models that are more sustainable
The panel was optimistic that data and technology would help reduce waste in healthcare systems and make healthcare more affordable and sustainable for the long term. Technology is facilitating a shift from paying for volume-based care to paying for outcomes. With electronic medical records, the ability to mine databases of real-world evidence of medicines and machine learning, it is now possible to assess which patients are most or least likely to benefit from specific drugs, and prescribe accordingly. Telemedicine enables a more optimal use of patient and physician time.
Technology also holds the promise of early diagnoses and preventative care, which could pre-empt costly interventions in late-stage diseases. For example, Grail’s Galleri liquid-biopsy test is able to detect 50 cancers at early stages with one blood draw. A combination of data and technology, new diagnostic tools, more effective treatment modalities and better application of resources could thus help make healthcare systems more sustainable over time.
Improving healthcare systems in underserved communities
Pharmaceutical companies now realise that simply donating medicine (e.g. for cancer) to poor countries does not work as they oftentimes lack the know-how and infrastructure to diagnose complex conditions and deliver specialty medicine. A more sustainable model is for pharma companies to invest and help these countries develop their own healthcare ecosystems. Remote training programmes were also highlighted as a way to increase access to specialty care in underserved areas. One example is Project ECHO, a global tele-mentoring programme where specialists in the developed world help upskill generalists in emerging countries into specialists, enabling better care for more people.
Click on “Save as PDF” to access the pdf version of the article.